General information
Autoimmune gastritis is an atrophic inflammation of the deep layers of the gastric mucosa, which is caused by autoimmune processes that occur in the patient's body.
Autoimmune gastritis is an atrophic inflammation of the deep layers of the gastric mucosa, which is caused by autoimmune processes that occur in the patient's body. This is the rarest type of gastritis. It occurs when the immune system recognizes cells of the parietal epithelium as pathogenic, to which antibodies are produced that attack the mucous membrane. This leads to increased secretion of hydrochloric acid in the stomach. The disease is more typical for the bottom and body of the organ, which is due to the large amount of lining epithelium in these areas.
It is believed that predisposition to the disease is genetically determined, and gastritis can also be triggered by diet, as with other types of disease.
Autoimmune gastritis: causes, symptoms and treatment
Autoimmune gastritis is a rare case in the practice of gastroenterologists.
This specific type of gastritis has not been fully studied. The mechanism of occurrence and development of this disease is complex, as in other cases of occurrence. Autoimmune gastritis, or gastritis type A, occurs only in 7–10% of cases, according to rough estimates by doctors. Type A gastritis is an autoimmune disease, the distinctive feature of which is the transient atrophy of the gastric mucosa, with the death of a large mass of cells. In such a case, the immune system perceives the cells of the gastric mucosa as foreign agents and begins to actively produce antibodies against them. Many doctors note that the disease is transmitted at the genetic level, becoming a consequence of genetic mutations. Antibodies produced by the immune system begin to fight gastromucoprotein, a secretion that protects the stomach from various inflammatory infections.
Gastritis type A
When an autoimmune process occurs, the bottom and body of the stomach are affected. As a result, the production of gastric juice and other important components involved in digestion is significantly reduced. With autoimmune gastritis, the development of vitamin B-12 deficiency is observed. The phenomenon is associated with a decrease in the content of the Castle factor in the body, which is responsible for the normal absorption of the vitamin.
Gastritis type A (autoimmune gastritis)
Type A gastritis is rare. Usually the fundus and body of the stomach are involved in the process; changes in the antrum are minor. This form of gastritis is often observed in Addison-Biermer disease.
In 90% of people suffering from Addison-Biermer disease, and in more than half of the remaining patients with type A gastritis, antibodies to parietal cells are found in the serum; in addition, antibodies to intrinsic Castle factor are often found. The presence of autoantibodies indicates the participation of autoimmune mechanisms in the pathogenesis of this form of gastritis. However, not all patients have autoantibodies, and in many of them the disease appears to be caused by Helicobacter pylori (type B gastritis).
Antibodies to parietal cells have a cytotoxic effect on the gastric mucosa. In relatives of people suffering from Addison-Birmer disease, antibodies to parietal cells, atrophic gastritis and hypochlorhydria are detected with increased frequency. Antibodies to parietal cells are found in 20% of people over 60 years of age and in approximately 20% of patients with autoimmune polyglandular syndrome type I. Antithyroid antibodies are detected in 50% of people with Addison-Biermer disease, and approximately 30% of people with thyroid disease have parietal cell antibodies. 40% of people with Addison-Biermer disease have antibodies to intrinsic factor. These antibodies are more specific for autoimmune gastritis than antibodies to parietal cells. It is possible that cellular immunity also plays a role in damage to the mucosa in Addison-Birmer disease.
In autoimmune gastritis, the gastric glands containing parietal cells are destroyed, and as a result, the secretion of hydrochloric acid is reduced.
In autoimmune gastritis, the gastric glands containing parietal cells are destroyed, and as a result, the secretion of hydrochloric acid is reduced. Since parietal cells also secrete intrinsic factor, autoimmune gastritis leads to impaired absorption of vitamin B12, megaloblastic anemia and neurological disorders.
The further the destruction of parietal cells and atrophy of the mucous membrane of the fundus and body of the stomach have gone, the more the secretion of hydrochloric acid is reduced. Sufferers of Addison-Birmer disease typically have achlorhydria, and serum gastrin levels are almost as high as in Zollinger-Ellison syndrome. Since the antral mucosa is relatively intact, G-cells continuously secrete gastrin (normally, its secretion is inhibited when the gastric contents become acidic). Sometimes significant hypergastrinemia leads to enterochromaffin-like cell hyperplasia and gastric carcinoids. The latter may undergo reverse development after removal of G-cells during anthrumectomy. Serum gastrin levels in autoimmune gastritis with achlorhydria or severe hypochlorhydria are increased even in the absence of Addison-Biermer disease.
In patients with autoimmune CG, herpes viruses are detected in the epithelial and stromal cells of the gastric mucosa by immunohistochemical research (cytomegalovirus infection in 100%, herpes simplex virus types 1 and 2 in 50% of patients; in 72% of patients, a combination of two and three viruses). An inverse correlation between herpes viruses and HP has been established: with an increase in the degree of contamination of the gastric mucosa with HP, the number of cells containing herpes viruses decreases, and with a decrease, it increases. A prospective five-year observation of 45 patients with autoimmune CH, associated and not associated with HP, was carried out, of which 27 patients with ACH. Treatment of patients with autoimmune CG with the drug Novobismol showed positive clinical, endoscopic and morphological dynamics: a decrease in the frequency and intensity of symptoms of gastric dyspepsia and signs of inflammatory activity.
Mechanisms of development of autoimmune gastritis
There are two types of autoimmune inflammation of the stomach:
- atrophic autoimmune gastritis;
- chronic autoimmune gastritis without atrophy.
In the first case, antibodies are produced to the cells of the inner lining of the stomach, which secrete hydrochloric acid and gastromucoprotein.
Gastromucoprotein (or intrinsic Castle factor) is a substance that protects the mucosa from damage and ensures the absorption of cobalamin (vitamin B12).
With this form of the disease, the secretion of hydrochloric acid quickly disappears and achlorhydria develops - a complete absence of hydrogen chloride in the stomach.
In such conditions, not only the digestive processes suffer, but also degeneration of the mucous membrane occurs. Destroyed cells are replaced by connective tissue and intestinal epithelium. As a result, after a few years, this leads to the formation of a malignant neoplasm - adenocarcinoma. The processes intensify against the background of hypergastrinemia.
Under conditions of increased pH of gastric juice, the body tries to reduce this indicator by increasing the production of gastrin, a hormone that stimulates the secretion of hydrochloric acid.
However, gastrin cannot affect the destroyed mucosal cells, and the pathological process progresses. According to official medical data, the likelihood of developing adenocarcinoma or carcinoid in patients with autoimmune gastritis is 2-4 times higher.
Another significant factor in the pathogenesis of autoimmune inflammation is the disruption of gastromucoprotein formation. Against this background, symptoms of B12 deficiency anemia develop, including disorders of the nervous system.
In chronic autoimmune gastritis without atrophy, antibodies are produced only to gastromucoprotein. Therefore, inflammation of the stomach develops due to a decrease in the protective functions of the intrinsic factor of Castle and is not accompanied by atrophy.
But the symptoms of anemia come to the fore, which we will discuss in more detail later. This form of autoimmune gastritis is characterized by a milder course and a favorable prognosis with adequate therapy.
Historical reference . Autoimmune gastritis with atrophy was first described by the English physician Thomas Addison in 1849. He identified this disease in a patient with severe anemia. However, the direct connection between anemia and gastritis was confirmed only in 1860, when antibodies to gastromucoprotein were discovered.
Course of the disease
With autoimmune gastritis, the human digestive system begins to eat itself. Like this? Strange processes are launched in the human body - the immune system begins to perceive the cells of the gastrointestinal tract as foreign. As a result, the acidity of the stomach decreases, food is not digested and begins to rot in the body, nutrients are not absorbed either into the general bloodstream or into the tissues of the body. After each meal, a person begins to experience uncomfortable painful sensations in the lower abdomen. As a result, patients consciously begin to refuse food because it hurts them to eat it. Over time, the patient develops dystrophy and anorexia (underweight).
Symptoms
The development of autoimmune gastritis negatively affects not only the digestive system, but also the cardiovascular system, and the functioning of the nervous system is often disrupted.
Symptoms of autoimmune gastritis are:
- nausea;
- vomit;
- stomach discomfort;
- heartburn;
- belching;
- feeling of heaviness after eating;
- unstable bowel movements;
- low blood pressure;
- frequent attacks of headache;
- a sharp decrease in body weight;
- dryness and flaking of the skin;
- deterioration of hair and nails;
- increased fatigue;
- irritability;
- insomnia.
It is worth noting that pain with autoimmune gastritis appears extremely rarely. Most often, the patient feels discomfort in the upper abdomen. When the first signs of disorders of the digestive system appear, it is necessary to seek help from a gastroenterologist, because the older the patient, the faster the disease progresses.
Causes and conditions of the disease
The exact etiology of this autoimmune disease has not been determined. Official medicine believes that chronic autoimmune gastritis has a genetic predisposition. The disease may be accompanied by other disorders of the gastrointestinal tract and endocrine system.
Provoking factors may be:
- weakened immunity;
- history of inflammatory and infectious diseases;
- stress;
- unhealthy diet;
- intemperance in drinking alcohol;
- smoking.
For your information! In the absence of individual predisposition, these circumstances in themselves cannot serve as the cause of the disease.
What is autoimmune gastritis and how serious is it?
Autoimmune gastritis is a rare inflammatory disease in which the body itself acts destructively on the mucous tissues of the stomach.
Autoimmune gastritis is a rare inflammatory disease in which the body itself acts destructively on the mucous tissues of the stomach. This condition is associated with malfunctions of the immune system. Autoimmune disease does not depend on the gender or age of the patient. This form of gastritis is diagnosed in approximately 1 case out of 10.
Forms of the disease
Most often, the disease develops immediately into a chronic form and is called type A gastritis in the classification of chronic gastritis, but sometimes the disease develops as an atrophic disease.
Atrophic
Autoimmune atrophic gastritis is inflammation of the mucous membrane in the stomach, which is caused by the fact that there are not enough glands in it to secrete substances necessary for digestion (secretory insufficiency) and problems with motility. When the immune system destroys many parietal cells, their complete restoration is impossible, which often becomes the cause of stomach cancer.
Chronic
Chronic autoimmune gastritis is more common than atrophic gastritis. It is characterized by the fact that relapses often occur, the absorption of nutrients in the organ is disrupted, and therefore persistent vitamin deficiency occurs. This affects the patient’s appearance (poor vision, skin, nails, hair loss, etc.). Chronic gastritis is localized in a specific area of the organ without affecting others. The disease has a dangerously high risk of complications.
Chronic autoimmune gastritis is more common than atrophic
heartburn;- unpleasant taste in the mouth;
- frequent belching with a bad odor;
- discomfort in the epigastrium after a meal;
- nausea;
- the intestines growl;
- flatulence;
- gagging;
- constipation gives way to diarrhea;
- my stomach hurts;
- distension in the stomach area.
With a long course of the disease, external signs appear.
Stages of exacerbation
Autoimmune gastritis with long-term development can manifest itself as follows:
- the desire to eat disappears;
- weight loss;
- the appearance of plaque on the tongue;
- sleep problems;
- prostration;
- headache;
- hyperhidrosis, which is associated with food intake;
- mood swings;
- dark spots;
- avitaminosis;
- dizzy;
- low pressure;
- problems with the cardiovascular system;
- bad nails, hair, teeth;
- severe pallor, etc.
Gastritis
Gastritis
Iron deficiency
8075 March 24
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Gastritis: causes, symptoms, diagnosis and treatment methods.
Gastritis is inflammatory and/or dystrophic changes in the gastric mucosa of various origins.
The stomach is a hollow muscular organ that is part of the digestive system.
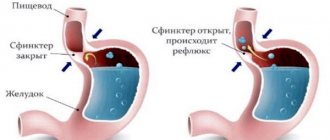
It is located between the esophagus and the duodenum, from which it is separated by circular muscles - sphincters, which ensure isolation of its contents. The stomach consists of several sections: cardiac (inlet), fundus (upper dome), body (central part), antrum and pyloric (outlet).
The gastric wall has four layers: mucous, submucosal, muscular and serous. The stomach performs several functions. It deposits (preserves) food for the time necessary for its primary processing; contraction and relaxation of its muscles (motility) provide mechanical processing of food. Cells of the gastric mucosa produce hydrochloric acid and digestive enzymes for the chemical processing of food, and participate in enhancing hematopoietic function through the production of a specific substance - internal Castle factor. The acid barrier of the stomach prevents the penetration of microorganisms into the underlying sections of the gastrointestinal tract, which manifests the protective function of this organ.
Inflammation of the gastric mucosa - gastritis - is a very common condition that occurs at any age. According to research, gastritis occurs in approximately half of the working population.
Causes of occurrence
Gastritis occurs due to an imbalance between processes that provide protection or cause damage to the gastric mucosa.
Acute
inflammation
is caused by short-term exposure to strong irritating factors.
These can be chemicals (for example, drugs, acids, alkalis), mechanical or thermal irritants (swallowed sharp objects, excessively hot/cold food or liquid), pathogens of foodborne toxic infections (salmonella, staphylococcus, etc.).
Severe stress, massive skin burns, myocardial infarction, etc. can provoke the formation of erosions (superficial defects of the mucous membrane) and stomach ulcers.
Chronic gastritis
is a disease that is characterized by a long process of changes in the structure of the gastric mucosa, up to the replacement of the mucous epithelium with scar tissue, as a result of which the function of the stomach is impaired.
Causes of chronic inflammation:
– the pathogenic bacterium Helicobacter pylori, which infects the middle and lower parts of the stomach, despite high acidity;
According to data from various regions of our country, H. pylori infection is found in 65–92% of adults, and therefore the issues of its diagnosis and treatment are extremely relevant. The high incidence of chronic Helicobacter gastritis causes a high incidence of other diseases associated with this bacterium (peptic ulcer of the stomach and duodenum, stomach cancer). – autoimmune pathologies, in which the immune system perceives the cells of the gastric mucosa as foreign and destroys them, which reduces the production of hydrochloric acid and digestive enzymes; – long-term use of non-steroidal anti-inflammatory drugs leads to a weakening of the synthesis of prostaglandins and a decrease in mucus production, which leads to damage to the gastric mucosa by hydrochloric acid; – reflux (duodeno-gastric) – backflow of duodenal contents into the stomach due to failure of the duodenal sphincter, which leads to inflammation and disruption of the gastric mucosa.
Risk factors for the development of chronic gastritis are bad habits (smoking, drinking alcohol), dietary errors (non-compliance with diet, an abundance of fried, spicy foods), hereditary predisposition, metabolic disorders, hormonal abnormalities, stress, etc. Classification of
the disease
Depending on Depending on the nature of the damage, the following types of acute gastritis are distinguished:
– catarrhal (simple) gastritis
characterized by inflammatory changes in the gastric mucosa, most often occurring with poor nutrition;
– fibrinous gastritis
develops in severe infectious diseases;
– corrosive gastritis
occurs when concentrated alkalis, acids and other toxic substances enter the stomach;
– phlegmonous gastritis
develops when bacteria and protozoa enter directly into the wall of the stomach, with traumatic injuries, as a complication of an ulcer or with stomach cancer.
Types of chronic gastritis:
– superficial non-atrophic gastritis
occurs due to colonization of the gastric mucosa by the bacterium Helicobacter pylori (type B gastritis);
– atrophic gastritis
, which can be
autoimmune
(type A gastritis) and
multifocal
(type A and B gastritis).
Special forms of chronic gastritis: medicinal
(while taking medications),
reactive reflux gastritis
(type C gastritis),
radiation
(occurs as a result of radiation therapy),
eosinophilic
(can develop in people with food and drug allergies).
Based on the source of inflammation, antral gastritis, gastritis of the body of the stomach or all parts of the stomach are distinguished - pangastritis.
Chronic gastritis can occur with a change in the production of hydrochloric acid towards an increase (hypersecretory) or decrease (hyposecretory), but in some cases the level of hydrochloric acid remains normal.
Chronic gastritis can be in remission or exacerbation.
Symptoms
Acute gastritis sharply disrupts the functioning of the stomach and is manifested by a complex of symptoms: pain in the epigastric region (upper central part of the abdomen between the ribs), vomiting (may be mixed with blood), belching, heartburn, and deterioration in general well-being.
With the infectious genesis of acute gastritis, a rise in body temperature and the occurrence of diarrhea are possible - signs of the spread of infection.
In case of poisoning with chemicals, severe pain occurs in the mouth, pharynx, esophagus, stomach, and there may be vomiting of blood and drooling. Due to damage and swelling of the upper respiratory tract, breathing becomes difficult.
Ingestion of foreign bodies may remain asymptomatic, especially if the object passed through the esophagus without damaging it. The only manifestation may be increased salivation. If a foreign body remains in the stomach, there may be direct damage to the gastric wall with the development of bleeding or, over time, a pressure sore of the stomach wall with the formation of a hole, which is a life-threatening condition.
Chronic gastritis develops gradually and is characterized by a slow increase in symptoms of dyspepsia - signs of impaired digestive function.
These include: a feeling of heaviness in the epigastric region during or immediately after eating, belching, heartburn, stool disorders, intolerance to certain foods, medications. There may be pain on an empty stomach, nausea, vomiting (including blood or bile), and changes in appetite. The listed symptoms occur in various combinations in certain forms of chronic gastritis.
It should be remembered that changes in the condition of the gastric mucosa may not be clinically apparent.
Diagnostics
Diagnosis of gastritis is based on collecting anamnesis, identifying the clinical picture, and a thorough examination of the patient.
To clarify the nature of damage to the mucous membrane, study the function of the stomach, and search for the causes of inflammation, the following laboratory and instrumental studies are used:
– reference methods for diagnosing H. Pylori infection, as the most common cause of chronic gastritis, are a breath test with 13C-labeled urea and a test for the presence of H. pylori antigen in stool;
What is included in the diagnosis of autoimmune gastritis?
The diagnosis of autoimmune gastritis includes a number of tests and studies. In particular, these are:
- General blood analysis;
- Deficiency of vitamin B12, B9 and a number of other vital vitamins necessary for the normal functioning of the body.
- Carrying out an immunogram - it will be necessary to check whether the human immune system really perceives the gastrointestinal tract as a foreign body. To do this, you will need to take tests in the laboratory: antibodies to the internal Castle factor, to galiadin, and also to stomach cells.
- A gastroenterologist must conduct an instrumental examination - gastroscopy. This will make it possible to understand how far the pathological process has gone and in what condition the gastric mucosa is currently located. To prescribe the correct and, most importantly, effective treatment, you need to know the state of the gastrointestinal tract.
Consequences
According to statistics, every sixth person with chronic gastritis suffers from its autoimmune form.
If you do not contact a medical facility in a timely manner, the disease leads to:
- Anemia is a condition in which the level of hemoglobin and red blood cells in the blood is significantly reduced.
- Deficiency of vitamin B12, which plays an important role in the process of hematopoiesis.
- Polyhypovitaminosis is a deficiency of several vital elements at once.
- Gastric adenocarcinoma is a malignant tumor, with metastases spreading very quickly to other organs. Every year, several hundred thousand people die from stomach cancer.
Diagnostics
A specialist can easily diagnose gastritis based on symptoms, but autoimmunity of the disease is more difficult to identify, so a detailed examination of the stomach is necessary. Examinations:
A specialist can easily diagnose gastritis based on symptoms, but autoimmunity of the disease is more difficult to identify, so a detailed examination of the stomach
(fibrogastroduodenoscopy) is necessary;- biopsy with histological analysis of the biopath;
- probing, which will help identify Helicobacter and the level of acid in the organ;
- immunological analysis;
- blood serum test for gastrin levels;
- general blood analysis;
- ultrasound examination of the abdomen.
The most important step in determining the autoimmunity of gastritis is fibrogastroduodenoscopy with biopsy.
Polymerase chain reaction (PCR)
PCR may be prescribed as an additional examination method. This study makes it possible to study the patient’s tissues for the presence of microorganisms that are components of DNA viruses.
Immunological analysis
Autoimmune disorders are detected using an immunological blood test. It allows you to identify many disorders and confirm the diagnosis in patients with autoimmune gastritis.
Gastrin level determination
This indicator is determined by blood serum analysis. An increase in the indicator is a signal that malignant degeneration of stomach tissue is possible.
Probing
In order to exclude the presence of Helicobacter and to determine the level of acidity, the patient undergoes gastric intubation.
This is a necessary, albeit unpleasant, procedure. In order to exclude the presence of Helicobacter and to determine the level of acidity, the patient undergoes intubation of the stomach. This is a necessary, albeit unpleasant, procedure.
Fibrogastroduodenoscopy with biopsy
The event is carried out to determine the condition of the gastric mucosa. Depending on the stage of the disease, the doctor notes the presence of swelling, erosions, the color of the mucous membrane, and the presence of deformities. A biopsy allows you to recognize cancer.
Completing diagnostic measures allows you to clarify the diagnosis, identify all the features of the condition and outline a treatment strategy for the disease.
Who prescribes treatment
The patient’s examination and further treatment are carried out by two specialists - an immunologist and a gastroenterologist. The immunologist must determine at what stage the pathological process is currently located and how further destruction and destruction of the gastrointestinal tract can be prevented.
The gastroenterologist treats the already damaged gastric mucosa; prescribes treatment aimed at restoring the functions of the gastrointestinal tract that have been impaired during the progression of the disease.
Choice of treatment method
Treatment of autoimmune gastritis cannot be general for all patients with this diagnosis. This is due to the fact that gastric damage is different in all patients. Therefore, therapy is prescribed exclusively on an individual basis.
In the first stages, the patient may be prescribed drugs such as: Cerucal, Motilium, No-Shpa, Drotaverine, Papaverine, Famotidine, Metacin. If the pathological process has affected the function of hydrochloric acid production, then natural gastric juice is prescribed to activate it and fully digest food. Since in the body of a patient diagnosed with “autoimmune gastritis” there is naturally a deficiency of B vitamins, folic acid, as well as a number of useful substances and microelements, then in this case you need to take a complex of vitamins and minerals. In some cases, gastritis treatment and maintenance therapy are carried out throughout the patient's life.
Traditional methods of treating autoimmune gastritis involve the use of plantain juice, as well as natural sea buckthorn oil. According to reviews of patients who used traditional medicine in treatment, unfortunately, there was no improvement in their well-being.
Treatment
The treatment regimen for autoimmune gastritis includes taking medications and adjusting the diet.
The gastroenterologist prescribes the following types of drugs:
- antispasmodics;
- painkillers;
- medications that normalize peristalsis;
- restoring the mucous membrane,
- enzymes.
In addition, taking multivitamin complexes is indicated.
Treatment of autoimmune gastritis should be accompanied by a strict diet for at least 2 weeks. It is recommended to eat only warm food with a puree-like consistency. Rough, cold or very hot food entering the body complicates the course of the disease.
Fatty, fried, spicy, sour, salty, smoked foods, baked goods, carbonated and alcohol-containing drinks must be excluded from the diet.
If all recommendations are followed responsibly, symptoms disappear after a few days.
Treatment and diet
It is completely impossible to cure this form of the disease, since the disease has not been fully studied, especially in the case of complete atrophy of the mucous membrane.
Therapy for the disease is prescribed only after a final diagnosis has been made. Treatment of autoimmune gastritis, like any type of disease, is complex. Goals:
- elimination of exacerbation;
- relieving inflammation;
- relief of symptoms;
- improving the functioning of the gastrointestinal tract.
- dietary nutrition;
- use of pharmaceuticals;
- balneotherapy;
- reflexology.
It is completely impossible to cure this form of the disease, since the disease has not been fully studied, especially in the case of complete atrophy of the mucosa. Therefore, it is important to start therapy before this happens. If complete destruction has occurred, the patient is recommended drugs that are included in replacement therapy; the patient takes medicinal analogues of enzymes (gastric juice, pepsin, etc.), for example, Abomin, Pepsidil, etc.
If the disease causes anemia, the patient needs to take a course of vitamin B12 and folic acid. If Helicobacter group bacteria are found in the stomach, you need to undergo treatment with antibacterial agents. But the use of antibiotics is not always necessary. Only a doctor can determine whether Helicobacter causes additional harm or not. The patient may also be prescribed the following medications:
- antispasmodics for pain relief (“No-Shpa”, “Papaverine”, “Drotaverine”);
- medications that improve peristalsis (“Cerucal”, “Metacin”);
- medications that help normalize the mucous membranes of the organ (Bismuth preparations);
- vitamin and mineral complexes or vitamins B12, folic acid.
Such maintenance therapy is often necessary throughout the patient's life. Treatment for each specific patient is selected individually, which depends on the degree and location of mucosal atrophy. Only after making an accurate diagnosis, the doctor determines how to treat the patient. Dietary nutrition is an important part of the treatment of gastritis, but it should be understood that it does not cure the disease, but helps reduce the load on the gastrointestinal tract by eliminating junk food and irritants. In the countries of the former USSR, the Pevzner diet is recommended.
Diet principles:
- fractional meals (small portions, weighing 200 g);
- eating schedule (you need to eat at the same time 5-6 times a day);
- food should be warm (not cold or hot);
- exclude rough, fatty, fried, spicy, salty, smoked foods from the diet;
- alcoholic drinks are prohibited;
- food needs to be steamed or boiled, sometimes you can bake it in the oven;
- It is better to grind food to the consistency of puree;
- caffeine-containing drinks will harm the stomach (coffee, tea);
- You should not eat sweets and chocolate.
Sometimes traditional medicine is used as an additional treatment. They can be taken only after consultation with your doctor. Fennel, thyme, plantain, and mint are considered useful plants for gastritis. Sea buckthorn oil has healing properties. For autoimmune gastritis, it is recommended to stop smoking, since tobacco smoke irritates the gastric mucosa.
Treatment of autoimmune gastritis
Clinical recommendations for the treatment of autoimmune gastritis include the following groups of medications:
- Natural gastric juice is a replacement therapy that replenishes the deficiency of hydrochloric acid and gastric enzymes.
- Enzyme preparations (Abomin, Pepsidil, Creon) that stimulate food digestion.
- Stimulants of digestive tract motility (Cerucal, Motilium) are prescribed to improve the evacuation of food from the stomach, especially indicated in the presence of nausea and vomiting.
- Antispasmodics (Buscopan, No-shpa, Papaverine) help relieve pain in the epigastrium.
- Bismuth preparations (De-nol, Visnol) have anti-inflammatory and astringent effects and help destroy Helicobacter pylori.
- When H. pylori is detected in the gastric contents, eradication therapy is prescribed with great caution, since in addition to antibiotics it includes drugs that suppress the secretion of hydrochloric acid. They are prescribed only after assessing the results of pH testing.
Dietary recommendations for autoimmune gastritis are not fundamentally different from the standard diet for chronic inflammation of the stomach. It is especially important to observe the temperature regime and not to abuse fatty, coarse fiber foods. For symptoms of hypovitaminosis, it is recommended to take vitamin-mineral complexes.
The treatment of B12-deficiency anemia deserves special attention. To correct it, cyanocobalamin is prescribed in injection form and drugs that stimulate the nervous system (Neuromidin, Mexidol, Actovegin).
Autoimmune gastritis is a disease that requires mandatory drug treatment. Especially in the later stages, when it is necessary to carry out replacement therapy with enzymes and natural gastric juice.
However, treatment should be started at the earliest stages of the disease. This will slow down its progression and with a high probability avoid malignant degeneration of the cells of the gastric mucosa.
How it develops
The development of an autoimmune process can be triggered by mechanical trauma to the gastric mucosa, which can be provoked by coarse food particles, its chemical irritating properties, and Helicobacter. If immunoglobulin type A is produced in insufficient quantities and “inadequate” antibodies are produced, instead of promoting healing of the mucous membranes, the immune system attacks the parietal cells.
At this time, antibodies to Castle factor are produced (an element of the stomach’s protective mechanism against infections), which causes problems with the absorption of vitamin B12. Such antibodies have a destructive effect on the mucous membrane of the organ (attack the glands), which over time leads to enzyme deficiency, since the glands that produce them are inhibited and atrophy. This leads to disruption of the digestion process and anemia. Autoimmune processes develop in the body and bottom of the stomach. It has not yet been precisely established whether mucosal atrophy is caused by the production of aggressive antibodies or vice versa.
Diet food
Diet is one of the components of treatment that should not be neglected.
The main approach to choosing dishes: they should not create increased stress on the gastrointestinal tract. Diet is one of the components of treatment that should not be neglected. The main approach to choosing dishes: they should not create increased stress on the gastrointestinal tract.
To do this, remove from the patient’s menu:
- cold, hot and rough food;
- spicy and fatty foods;
- fresh baked goods, sweets;
- hard-to-digest and rough food, including smoked meats.
Advice! It is advisable to give up bad habits.
Preference should be given to food with a soft consistency and warm temperature. Steamed, boiled and baked dishes will be best digested.
To stabilize the condition, it is important to follow a meal schedule. Eat small portions 5-6 times a day.
Complete cure of autoimmune gastritis is impossible due to the specificity of the disease and unknown origin, especially with atrophy of the gastric mucosa. In this regard, it is extremely important for a favorable prognosis to follow the instructions of the attending physician, follow the specified treatment regimen, follow a diet and regularly monitor the condition.
Prevention
Due to the fact that the pathology does not have an exact cause, there are no special preventive measures. People should adhere to the general rules for the prevention of gastritis, which include:
- timely treatment of all gastrointestinal diseases;
- eliminating bad habits;
- proper nutrition.
Compliance with such recommendations makes it possible, if not to exclude, then to significantly reduce the risk of developing this disease.
Sources:
https://empendium.com/ru/chapter/B33.II.4.5.3.https://www.med-sovet.pro/jour/article/view/333?locale=ru_RUhttps://gastritinform.ru/ medbiol.ru/medbiol/har3/000dbde9.htmhttps://gastritinform.ru/private-catering.ru/autoimmunnyj-gastrit-atroficheskij/https://okgastro.ru/zheludok/264-autoimmunnyj-gastrithttps://medportal. su/autoimmunnyj-gastrit-prichiny-simptomy-lechenie/