Treatment of gastric and duodenal ulcers requires an integrated approach. During therapy, several groups of medications are used at once. Some of them are recommended for use in tablet form, but others are administered by injection or through droppers. The main goal of drug treatment is to return the disease to a stage of stable remission.
Restoring the stomach and duodenal mucosa after an exacerbation of peptic ulcer disease through the use of folk remedies and methods of alternative medicine will not give the desired result. It is possible that the patient’s general well-being may deteriorate.
Medicines for stomach and duodenal ulcers are represented by the following groups:
- antibacterial drugs;
- histamine receptor blockers;
- proton pump inhibitors;
- gastroprotectors;
- anticholinergics;
- antacids;
- antiemetics;
- antispasmodics.
Antibacterial drugs
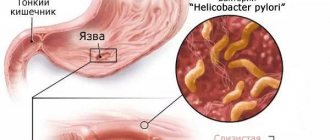
Medicines from the group of antibiotics help destroy Helicobacter pylori, the main causative agent of gastritis and peptic ulcers. Most often, it is this bacterium that causes the development of the disease.
Important! They can be prescribed in tablet or injection form.
Treatment is carried out using the following drugs.
- Clarithromycin. The main antibiotic prescribed during an exacerbation of an ulcer. It is resistant to the acidic environment of the stomach, is slowly absorbed and has a long elimination period. Most often, a two-time dose is recommended. Duration of treatment – 6…14 days.
- Amoxicillin. Semi-synthetic antibiotic. Quickly penetrates into affected tissues. Has a bactericidal effect.
- Metronidazole. It has antimicrobial and antiprotozoal effects. Contraindications for use: hypersensitivity to the active component, organic damage to the central nervous system, liver failure.
- Tetracycline. Antibiotics with antimicrobial action. Intended for systemic use. It has a negative effect on the microflora of the stomach and gastrointestinal tract as a whole. During therapy, the formation of dysbiosis and other disorders is possible.
Causes of the disease
Doctors believe that the mechanism for the development of damage to the duodenum is triggered by certain types of the bacterium Helicobacter pylori. It is these tiny organisms that produce substances that influence the development of ulcers. The bacterium can survive in highly acidic environments, and ultimately provoke the development of stomach disease. The disease can make itself felt a couple of months or even years after the microorganism gets inside. Helicobacter pylori is killed during treatment with antibiotics.
There are other factors that can trigger this disease:
- hereditary predisposition;
- eating spicy, sour, fatty, canned, salty and pickled foods, as well as eating disorders;
- frequent stress and negative emotional stress;
- bad habits, in particular alcohol and cigarettes;
- errors when taking medications (antibiotics, non-steroidal anti-inflammatory drugs (NSAIDs), hormonal drugs, etc. have an irritating effect - these are so-called drugs that have ulcerogenic (ulcer-forming) properties).
Histamine receptor blockers
These ulcer tablets are mandatory. The drugs reduce the production of hydrochloric acid in the stomach by reducing the activity of the glands. Taking the drug temporarily blocks the parietal cells of the stomach, whose task is to produce digestive enzymes. As a result, there is a decrease in the inflammatory process, due to a decrease in the aggressive effect of gastric juice on the damaged mucous surfaces of the organ.
The following appointments are scheduled:
- Ranitidine. The drug blocks the functioning of H2 receptors in parietal cells, inhibits the production of hydrochloric acid, and reduces the level of pepsin in gastric juice. The antisecretory effect helps create favorable conditions for the healing of ulcers.
- Nizatidine. It has the ability to completely stop the secretion of digestive enzymes and gastric juice for up to 12 hours, which promotes active healing of the surfaces of ulcers. After taking the drug, the patient is only allowed to drink.
- Roxatidine. In terms of its effect, the drug is close to Nizatidine, but belongs to the group of independent blockers, since it has the ability to regulate the pH level of gastric juice.
- Famotidine. While taking the blocker, the production of gastric juice completely stops. Treatment with the drug can be carried out exclusively with medications that reduce the level of acidity of gastric juice.
- Cimetidine. Has a pronounced antiulcer effect. While taking the medicine, the production of hydrochloric acid is suppressed, the pH level of gastric juice increases, which significantly reduces the activity of pepsin. Cimetidine therapy helps restore the protective mechanisms of the gastric mucosa and heal existing damage. Duration of action – no more than 6 hours.
Modern approaches to the treatment of gastric and duodenal ulcers
Controlling stomach acid production is the cornerstone of peptic ulcer treatment. The classic formula of the early 20th century “no acid - no ulcer” has not lost its relevance; the most effective groups of drugs, according to their mechanism of action, are aimed at combating acidity. Antacid drugs Antacid drugs have been known since ancient times. This is a group of drugs that reduce the acidity of gastric contents through chemical interaction with acid in the stomach cavity. Currently, preference is given to non-absorbable antacids, which are relatively insoluble salts of weak bases. Non-absorbable antacids usually contain a mixture of aluminum hydroxide and magnesium hydroxide (Almagel, Maalox) or are aluminum phosphate (Phosphalugel). Unlike absorbable antacids (soda), they have much fewer side effects. They interact with hydrochloric acid, forming non-absorbable or poorly absorbed salts, thereby increasing the pH inside the stomach. At a pH greater than 4, pepsin activity decreases and it can be adsorbed by some antacids. Acid production in duodenal ulcers ranges between 60 and 600 mEq/day, in two thirds of patients - between 150 and 400 mEq/day. The total daily dose of antacids should be in the range of 200-400 mEq for neutralizing ability, for gastric ulcers - 60-300 mEq. Deciphering the mechanism of parietal cells and the regulation of acid secretion has made it possible to create new classes of drugs. The secretion of hydrochloric acid is under the stimulatory control of three classes of parietal cell receptors: acetylcholine (M), histamine (H2), gastrin (G) receptors. The path of pharmacological action on muscarinic receptors turned out to be historically the earliest. Non-selective M-anticholinergic blockers (atropine) and selective M1-antagonists (pirenzepine) have lost their importance in the treatment of peptic ulcers with the progress of drugs of other classes that act at the molecular level, interfere with intimate intracellular processes and provide a more powerful antisecretory effect. Histamine H2 receptor blockers Clinical studies have shown that there is a direct relationship between ulcer healing and the ability of drugs to suppress acidity. Ulcer healing is determined not only by the duration of administration of antisecretory agents, but also by their ability to “hold” intragastric pH above 3 for a given time. The meta-analysis made it possible to establish that a duodenal ulcer will heal within 4 weeks in 100% (!) of cases if the intragastric pH is maintained above 3 for 18-20 hours during the day. Despite the fact that patients with gastric ulcer have moderate levels of gastric secretion, antisecretory therapy is mandatory for them as well. Gastric ulcers are characterized by slower healing than duodenal ulcers. Therefore, the duration of prescription of antisecretory drugs should be longer (up to 8 weeks). It is assumed that we can expect scarring of gastric ulcers in 100% of cases if intragastric pH is maintained above 3 for 18 hours a day for about 8 weeks. Such control of acid secretion was achieved thanks to blockers of histamine H2 receptors in parietal cells. These drugs significantly influenced the course of peptic ulcer disease: the duration of ulcer scarring was reduced, the frequency of ulcer healing increased, and the number of complications of the disease decreased. Ranitidine for exacerbation of peptic ulcer is prescribed at a dose of 300 mg per day (once in the evening or 2 times a day, 150 mg), for duodenal ulcers, usually for 4 weeks, for gastric ulcers for 6-8 weeks. To prevent early relapses of the disease, it is advisable to continue taking a maintenance dose of ranitidine 150 mg/day. Famotidine (Quamatel) is used in a lower daily dose than ranitidine (40 and 300 mg, respectively). The antisecretory activity of the drug is more than 12 hours with a single dose. Famotidine is prescribed at a dose of 40 mg for the same duration as ranitidine. To prevent relapses of gastric ulcer – 20 mg/day. Histamine H2 receptor blockers are of particular importance in the treatment of bleeding from the upper gastrointestinal tract. Their effect is due to inhibition of hydrochloric acid production and an indirect decrease in fibrinolysis. In case of massive bleeding, drugs with parenteral forms of administration (Kvamatel) have an advantage. The effectiveness of histamine H2 receptor antagonists is due primarily to their inhibitory effect on acid secretion. The antisecretory effect of cimetidine lasts up to 5 hours after taking the drug, ranitidine - up to 10 hours, famotidine, nizatidine and roxatidine - 12 hours. Proton pump inhibitors A new step in the creation of antisecretory drugs has become inhibitors of H+,K+-ATPase of parietal cells - the enzyme that actually ensures the transfer of hydrogen ions from the parietal cell into the lumen of the stomach. These benzimidazole derivatives form strong covalent bonds with the sulfhydryl groups of the proton pump and permanently disable it. Acid secretion is restored only when new H+,K+-ATPase molecules are synthesized. The most powerful drug inhibition of gastric secretion today is provided by this group of drugs. This group includes drugs: omeprazole (Gastrozole), pantoprazole, lansoprazole and rabeprazole. Benzimidazole derivatives maintain pH values in a range favorable for the healing of gastric or duodenal ulcers for a long period of time in 1 day. After a single dose of a standard dose of a proton pump inhibitor, the pH above 4 is maintained for 7-12 hours. The consequence of such an active reduction in acid production is the amazing clinical effectiveness of these drugs. Data from numerous clinical trials regarding omeprazole therapy are shown in Table 2. Anti-Helicobacter therapy In parallel with the development of the latest generation of antisecretory drugs, scientific data and clinical experience were accumulated, which indicated the decisive importance of the Helicobacter pylori organism in the pathogenesis of peptic ulcer disease. Treatment that kills H. pylori is effective not only in healing the ulcer, but also in preventing recurrence of the disease. Thus, the strategy for treating peptic ulcer disease by eradicating H. pylori infection has an undeniable advantage over all groups of antiulcer drugs: this strategy provides long-term remission of the disease, and possibly a complete cure. Anti-Helicobacter therapy has been well studied in accordance with the standards of evidence-based medicine. A large number of controlled clinical trials provide grounds for confident use of certain eradication regimens. The clinical material is extensive and makes it possible to conduct meta-analysis. I will cite the results of just one of the meta-analyses conducted under the auspices of the US Food and Drug Administration: RJ Hopkins et al. (1996) concluded that in case of duodenal ulcer after successful eradication of H. pylori, relapses during long-term observation occur in 6% of cases (compared to 67% in the group of patients with persistent bacteria), and in case of gastric ulcer - in 4 % of cases versus 59%. Modern approaches to the diagnosis and treatment of H. pylori infection, meeting the requirements of evidence-based medicine, are reflected in the final document of the conference, which took place in Maastricht on September 21-22, 2000. For the second time, the European Helicobacter pylori Study Group organized an authoritative meeting to adopt modern guidelines on the problem of H. pylori. The first Maastricht Agreement (1996) played a significant role in regulating the diagnosis and treatment of H. pylori in the European Union. Over the past 4 years, significant progress has been made in this area of knowledge, which has forced the updating of previous recommendations. The Second Maastricht Agreement puts gastric ulcer and duodenal ulcer in first place among the indications for anti-helicobacter therapy, regardless of the phase of the disease (exacerbation or remission), including their complicated forms. It is especially noted that eradication therapy for peptic ulcer disease is a necessary therapeutic measure, and the validity of its use in this disease is based on obvious scientific facts. Indeed, eradication of H. pylori infection radically changes the course of the disease, preventing its relapse. Anti-Helicobacter therapy is accompanied by successful healing of the ulcer. Moreover, the ulcer-healing effect is due not only to the active antiulcer components of eradication regimens (for example, proton pump inhibitors or ranitidine bismuth citrate), but also to the actual elimination of H. pylori infection, which is accompanied by the normalization of the processes of proliferation and apoptosis in the gastroduodenal mucosa. The Second Maastricht Agreement emphasizes that in uncomplicated duodenal ulcers there is no need to continue antisecretory therapy after a course of eradication therapy. A number of clinical studies have shown that after a successful eradication course, ulcer healing actually does not require further medication. It is also recommended to diagnose H. pylori infection in patients with peptic ulcer disease who are receiving maintenance or course therapy with antisecretory drugs, with the prescription of antibacterial treatment. Carrying out eradication in these patients provides a significant economic effect due to the cessation of long-term use of antisecretory drugs. The outcome document of the 2000 Maastricht conference suggested for the first time that treatment for H. pylori infection should be planned without excluding the possibility of failure. Therefore, it is proposed to consider it as a single block, providing not only first-line eradication therapy, but also in case of persistence of H. pylori - second line at the same time (Table 3). It is important to note that the number of possible anti-helicobacter therapy regimens has been reduced. For triple therapy, only two pairs of antibiotics are offered; for quadruple therapy, only tetracycline and metronidazole are provided as antibacterial agents. First-line therapy: Proton pump inhibitor (or ranitidine bismuth citrate) at a standard dose 2 times a day + clarithromycin 500 mg 2 times a day + amoxicillin 1000 mg 2 times a day or metronidazole 500 mg 2 times a day. Triple therapy is prescribed for at least 7 days. The combination of clarithromycin with amoxicillin is preferable to clarithromycin with metronadzole, as it can help achieve a better result when prescribing second-line treatment - quadruple therapy. If treatment is unsuccessful, second-line therapy is prescribed: Proton pump inhibitor at a standard dose 2 times a day + bismuth subsalicylate/subcitrate 120 mg 4 times a day + metronidazole 500 mg 3 times a day + tetracycline 500 mg 4 times a day. Quadruple therapy is prescribed for at least 7 days. If bismuth preparations cannot be used, triple treatment regimens based on proton pump inhibitors are proposed as a second course of treatment. If the second course of treatment fails, further tactics are determined on a case-by-case basis. The treatment regimen of proton pump blocker + amoxicillin + nitroimidazole derivative (metronidazole) was excluded from the recommendations of the Second Maastricht Agreement. This combination is common in Russia, where metronidazole, due to its low cost and “traditional” use as a “reparant” for peptic ulcer disease, is an almost unchanged anti-Helicobacter agent. Unfortunately, in the presence of a H. pylori strain resistant to nitroimidazole derivatives, the effectiveness of this treatment regimen is significantly reduced, which has been proven not only in European studies, but also in Russia. Based on the results of a randomized controlled multicenter study, the purpose of which was to evaluate and compare the effectiveness of two triple therapy regimens: 1) metronidazole, amoxicillin and 2) omeprazole and azithromycin, amoxicillin and omeprazole in the eradication of H. pylori infection during exacerbation of duodenal ulcer. Eradication of infection in the group receiving metronidazole 1000 mg, amoxicillin 2000 mg and omeprazole 40 mg per day for 7 days was achieved in 30% of cases (confidence interval for the 95% probability was 17%-43%). We can only join the opinion of our European colleagues who excluded this scheme from the recommendations. Unfortunately, eradication therapy for H. pylori infection is not 100% effective. Not all provisions of the Second Maastricht Agreement can be unequivocally agreed with and without thoughtful analysis they can be transferred to our country. Bismuth-based eradication therapy regimens are currently not very widely used in Europe. However, the frequency of use of bismuth preparations in H. pylori eradication regimens varies across countries and continents. In particular, in the United States, triple therapy regimens containing bismuth are used to treat about 10% of patients. In China, regimens with a bismuth preparation and two antibiotics are in first place in terms of frequency of prescription. In his editorial in the European Journal of Gastroenterology and Hepatology, Wink de Boer (1999) rightly noted that “bismuth-based triple therapy is perhaps the most widely used in the world, as it is the only anti-Helicobacter therapy that is effective and economically accessible in developing countries.” countries of the world in which the majority of the world's population is concentrated.” Bismuth is also recommended for widespread use in the treatment of H. pylori infection in children. In Russia, the most widely used bismuth preparation is colloidal bismuth subcitrate (De-nol); Research is being conducted to determine the effectiveness and safety of eradication regimens using it. In 2000, the results of a study conducted by the Russian group studying H. pylori were published. In this study, eradication therapy included colloidal bismuth subcitrate (240 mg 2 times a day) + clarithromycin (250 mg 2 times a day) + amoxicillin (1000 mg 2 times a day). The duration of therapy was 1 week, eradication of H. pylori was achieved in 93% of patients. A list of other possible regimens, based on data from various clinical trials, is given in Table 4. Anti-Helicobacter therapy needs to be improved, and these recommendations are essential for its optimization. Antibiotics specifically directed against H. pylori, probiotics and vaccines may be included in the arsenal of anti-Helicobacter therapy in the future, but at present these drugs and treatment approaches are under development, and practical recommendations do not exist. Some new antibacterial drugs are of great interest, which have every chance of soon taking their rightful place in generally accepted eradication therapy regimens. A good example to illustrate the possibilities of optimizing a triple therapy regimen is azithromycin, a new drug from the macrolide group. Macrolide antibiotics, presented in triple eradication regimens mainly with clarithromycin, are perhaps the most effective. Therefore, azithromycin has been tried for a number of years as one of the possible components of therapy, but in early studies a relatively low dose of the drug was used. Increasing the course dose to 3 g led to an increase in the effectiveness of the standard seven-day triple regimen based on a proton pump inhibitor to the required level of more than 80%. In this case, the undoubted advantage is that as part of a weekly course, the full dose of azithromycin is taken over three days, once a day. This is convenient for the patient and reduces the percentage of side effects. In addition, in Russia the cost of azithromycin is lower than that of other modern macrolides. Ributin, a derivative of rifamycin S, has demonstrated very high activity against H. pylori in vitro. In combination with amoxicillin and pantoprazole, ributin led to 80% eradication in patients treated at least twice (!) with a standard triple regimen. Despite the fact that the reputation of nitroimidazoles is “tarnished” due to the high percentage of H. pylori strains resistant to them, research into this group of drugs continues. In in vitro experiments, the new nitroimidazole, nitazoxanide, proved to be highly effective against H. pylori, and the development of secondary resistance was not observed. In vivo studies should show how this drug can compete with metronidazole. As an alternative to multicomponent schemes, several approaches were theoretically offered for a long time, for example, the drug blockade of Ureaza - an enzyme, without which the existence of a bacteria is impossible, or the blockade of adhesion of microorganism to the surface of the epithelial cells of the stomach. The drug inhibiting urease has already been created, its activity in laboratory studies is indicated, including in relation to the enhancement of the effect of antibiotics used in anthelicobacter therapy. H.Pylori adhesions, such as rebepide or ekabeth, have been examined in combination with traditional anthelicobacter drugs. They statistically reliably increased the percentage of eradication compared to the same scheme without mucoprotective support. The use of double therapy (proton pump inhibitor + amoxicillin) was refused due to low efficiency, and the connection of a rebepide or ecabeth significantly increases the percentage of infection eradication. When the strains with the phenomenon of polyuretinity, stable both to the metronidazole and to clarithromycin, the combination of ecabet or rebuben with double therapy can become the treatment of the choice of choice. Opportunities that can discover a successful human vaccination against H.Pylori infection is difficult to evaluate due to their scale. Successes in the field of creating a vaccine allow us to hope that vaccination will be available in the coming years. The tested vaccines in animal experiments protect them from H.Pylori infection and related species of the Helicobacter genus, and in some cases lead to the elimination of microorganism. It was established that for successful immunization several H.Pylori antigens are needed. Due to the complete decoding of the microorganism genome, the selection of these antigens is greatly simplified. In addition, a number of studies are aimed at improving the adyuvant system, which is essential for improving the tolerance of the vaccine.
Aluminum hydroxide + magnesium hydroxide – Almagel (trade name) (Balkanpharma)
Omeprazole–Gastrozole (trade name) (ICN Pharmaceuticals)
Colloidal bismuth subcitrate – De-nol (trade name) (Yamanouchi Europe)
Famotidine–Kvamatel (trade name) (Gedeon Richter)
Proton pump inhibitors
Drugs in this group have the ability to temporarily stop the production of hydrochloric acid. The following drugs are used in the treatment process.
Lansoprozole
Inhibits the process of hydrochloric acid production. Does not slow down digestion. Prescribed before meals.
Omeprazole
The effect of Omeprazole begins within an hour after taking the dose. The effect lasts throughout the day. The drug suppresses the synthesis of hydrochloric acid and prevents increased secretion after eating.
Rabeprazole
Proton pump inhibitor with antibiotic properties. The product not only reduces the rate of production of digestive juice, but also destroys Helicobacter pylori. A single dose of Rabeprozole provides stomach protection for the next 48 hours.
Esomeprazole (analogue of Omeprazole)
Used in the developing stage of the disease. In the later stages it is ineffective.
Causes of disorders leading to the development of the disease
- hereditary predisposition - in such patients an increased number of cells responsible for the synthesis of hydrochloric acid was found; this leads to its production in large quantities when exposed to provoking factors;
- the microorganism Helicobacter pylori, which infects goblet cells responsible for mucus secretion and causes inflammation;
- long-term use of non-steroidal anti-inflammatory drugs and glucocorticoids (both simultaneously and separately), which leads to a decrease in mucus production; as a result, the walls of the organ become vulnerable to the effects of enzymes, hydrochloric acid and pancreatic juice;
- smoking and alcohol - nicotine stimulates the formation of hydrochloric acid and impairs blood circulation, and alcohol destroys the gastric mucosa;
- frequent stress – this increases motor skills and increases the production of hydrochloric acid;
- Among the rare causes are diseases in which the development of an ulcerative process in the gastrointestinal tract is possible: hyperthyroidism, Zollinger-Elisson syndrome.
Gastroprotectors
Gastroprotectors are a mandatory part of drug therapy for ulcerative pathology. After taking the drug, a protective layer is formed on the surface of the mucosa. Most often, the active substance is bismuth salts.
Gastroprotectors – a group of drugs used in the treatment of peptic ulcers
The following medications are prescribed for use. Venter. A product with a pronounced antiulcer effect. The active ingredient is sucralfate. While taking the medicine, there is an increase in the synthesis of gastric mucus, which helps reduce the aggressive effects of salts and acids. The drug is prohibited during gestation and breastfeeding. Among the side effects, it is worth highlighting a decrease in saliva production, nausea, and intestinal upset.
De-Nol. Gastroprotector with regenerating properties. The active ingredient is bismuth salt. The duration of treatment is four to eight weeks. Contraindications to treatment are poor kidney function, gestation and subsequent breastfeeding. The most common side effects are nausea and diarrhea.
Solcoseryl. Emergency medicine. Intended for intramuscular administration or intravenous infusion. There are few contraindications, but the development of an allergic reaction is possible.
Misoprostol (prescription drug). An antisecretory agent designed to reduce the amount of hydrochloric acid and digestive enzymes produced. The dosage regimen and dosage are determined individually by the attending physician. Contraindications for use are kidney and liver diseases, inflammatory processes in the gastrointestinal tract (GIT).
Methyluracil. A product that improves tissue trophism. For peptic ulcers, it is taken in a 40-day course. Side effects include headaches and dizziness.
Antisecretory agents for ulcers
Scientists have found that existing mucosal defects are scarred if the pH of at least 3 is maintained in the stomach and duodenum for 24 hours. For this purpose, drugs of three groups are used, each of which we will consider in more detail below.
Proton pump inhibitors (PPIs)
These are basic therapy medications that have an analgesic effect, reduce the symptoms of dyspepsia and accelerate the process of tissue scarring. Adverse reactions to taking inhibitors are in most cases mild and go away on their own. From the gastrointestinal tract, diarrhea or, conversely, constipation, flatulence and pain may occur.
Negative effects may affect the central nervous system. Thus, headache and dizziness are observed. Do not forget about the appearance of an allergic reaction, for example, itching, urticaria and Quincke's edema.
Recommended drugs in this group:
- Omeprazole. After consuming a single dose, the secretion of hydrochloric acid drops within the first hour, and after two hours it reaches its maximum. Take it in the morning before breakfast with a glass of water. The daily dose is 20-40 mg, and the course of treatment lasts 2-4 weeks;
- Lansoprazole. The patient receives the maximum amount of benefit after a couple of hours. You need to take it 1-2 times a day before meals. The daily dosage is 15-30 mg per day. Lansoprazole is prescribed after endoscopy.
- Pantoprazole. In addition to antisecretory, such tablets have an antibacterial effect. The duodenum and stomach are scarred in 88% of patients after 4 weeks of treatment. The daily norm is 40 or 80 g, and the duration of treatment is 14-28 days. Long-term use is not recommended, as complications may occur.
H2-histamine blockers
They slow down the production of hydrochloric acid and suppress the activity of pepsin. They act within 8-12 hours after consumption.
If the duodenum and stomach have scars, then the following is usually prescribed:
- Famotidine. Absorbed into the blood by 40-45%, and excreted through the kidneys. Begins to act in an hour. Pregnant and breastfeeding women, as well as those with cirrhosis, should not take this drug. They take 20-160 mg, and the duration of treatment is 4-8-12 weeks;
- Ranitidine. A similar drug that should be taken 300 mg in 1-2 doses.
Antacids
Of this group, the most popular are bismuth preparations, when used, the duodenum and stomach are covered with a protective film, causing an antacid, antimicrobial and anti-inflammatory effect. They remove excess stomach acid and reduce the activity of enzymes that aggravate the patient's condition. Examples include the following products: De-nol, Vis-nol and Bismuth nitrate. Take orally half an hour before meals with a glass of water. Antacids for gastric ulcers should be taken 480 mg per day, divided into 2-4 times.
Anticholinergics
In this group of medications, the most commonly prescribed medications are:
- Gastrocepin. Synthetically produced drug. Does not affect the functioning of the myocardium, salivary and sweat glands. During treatment, there is a decrease in the activity of receptors in the gastric mucosa, which is expressed in a decrease in the volume of pepsin.
- Buskopan. Blocks the processes of choline production in the stomach. It does not have a negative effect on other organs. At the same time, it has an analgesic effect.
- Platyfillin. It has a vasodilator, antispasmodic and sedative effect. Blocks cholinergic receptors. In large dosages, it inhibits gastric secretion. Side effect: tachycardia.
Antacids
This group of medications is used as enveloping, antiseptic and absorbent agents. They have the following properties: they remove toxic components and reduce the activity of digestive enzymes and hydrochloric acid.
Almagel and Maalox are commonly prescribed types of antacids
To protect the gastric mucosa, the following are used:
- Almagel. Forms a protective film on the surface of the mucosa. Effective at the beginning of the formation of ulcerative pathology. It has an analgesic effect, stimulates healing, and slows down the proliferation of pathogenic microflora.
- Maalox. Once the drug enters the stomach, it reduces acidity levels and also leads to a physiological normal level of acid-base balance. It has no direct effect on existing damage to the mucous membrane.
- Gastal. Short-acting antacid: the effect after administration lasts no more than two hours. Used in conjunction with drugs that become ineffective at high acidity levels of gastric juice.
- Phosphalugel. The product starts working quickly. Recommended for the relief of pain characteristic of the period of exacerbation of ulcerative pathology.
Drugs that reduce the aggressiveness of gastric juice
Drug treatment of stomach and duodenal ulcers is not possible without drugs that act on gastric juice, reducing its aggressiveness. There are several groups of such drugs.
Peripheral M-anticholinergics and calcium channel blockers
Peripheral M-anticholinergics block all subtypes of M-cholinergic receptors. Previously, these medications were often used to treat ulcers (Atropine sulfate, Pirenzepine), but in recent years they have been used less frequently. Although they have antisecretory properties, the effect is much lower, but there are many side effects. Calcium channel blockers are also rarely used. These are drugs such as Verapamil, Nifedipine. But if the patient has not only an ulcer, but also heart disease, the doctor may prescribe these medications.
H2-histamine receptor blockers
For stomach and duodenal ulcers, doctors often prescribe H2 receptor blockers, which have been used in medicine for more than 20 years. During this time, these drugs were well studied, doctors could not help but notice that it had become easier to treat ulcers. Thanks to the fact that these drugs began to be used, the percentage of scarring of ulcers became greater, the number of operations that had to be performed due to complications of the disease was reduced, and the treatment time was significantly reduced.
Another advantage of these drugs is that they increase the formation of mucus and improve microcirculation of the mucous membrane. However, these drugs cannot be abruptly discontinued, otherwise the patient may experience withdrawal syndrome, which will lead to increased acid secretion and relapse of the disease.
Generations of H2-histamine receptor blockers
There are several generations of H2-histamine receptor blockers.
- First generation. Cimetidine. It only lasts 4-5 hours, so you need to take this medicine at least 4 times a day. It has many side effects, for example, it affects the liver and kidneys. Therefore, now these tablets are practically not used.
- Second generation. Ranitidine. They last longer, 8-10 hours, and have fewer side effects.
- Third generation. Famotidine. One of the best drugs, it is 20-60 times more effective than cimetidine and 3-20 times more active than rantidine. Must be taken every 12 hours.
- Fourth generation. Nizatidine. Not much different from Famotidine, there are no special advantages over other drugs.
- Fifth generation. Roxatidine. It is slightly inferior to Famotidine; it has less acid-suppressing activity.
Proton pump inhibitors
These medications block the production of hydrochloric acid. They are much more effective than H2 receptor blockers, which is why these medications are often prescribed for peptic ulcers.
- Omeprazole. This medicine helps the ulcer heal faster. After 2 weeks of treatment, duodenal ulcers are scarred in 60% of patients, and after 4 weeks – in 93%. If you treat a stomach ulcer with Omeprazole, then after 4 weeks it will scar in 73% of patients, and after 8 weeks – in 91%.
- Lanzoprazole. The patient should take 1 capsule for two or four weeks for duodenal ulcers and up to 8 weeks for gastric ulcers. This medicine should not be taken by pregnant women, nursing mothers or those with a cancerous tumor in the gastrointestinal tract.
- Pantoprazole. You should not take this drug if you have hepatitis or cirrhosis of the liver. The recommended dose is from 40 to 80 mg per day, the course of treatment lasts 2 weeks for exacerbation of duodenal ulcer and 4-8 weeks for exacerbation of gastric ulcer.
- Esomeprazole. It is used to treat duodenal ulcers (20 mg 1 week, taken with antibiotics to get rid of Helicobacter pylori) and as a prophylactic for stomach disease (also 20 mg 1 time per day for 1-2 months with long-term use of NSAIDs ).
- Paries. This is a modern medicine that rarely has side effects, moreover, it has a more persistent antisecretory effect, so heartburn and pain will disappear on the first day of treatment.
Antacids
Antacids neutralize hydrochloric acid, which is part of the gastric juice. They are often prescribed for ulcers as an additional remedy. They help relieve pain and also reduce the intensity of heartburn. These drugs act quickly, much faster than other drugs, but they have a shorter therapeutic effect.
- Almagel. Contains magnesium hydroxide and aluminum hydroxide. The medicine envelops the stomach and protects its walls; it is also an adsorbent. Cannot be used for Alzheimer's disease and liver diseases. If the patient has a duodenal ulcer or stomach ulcer, you need to drink this remedy between meals, 1 spoon up to 4 times a day. The course of treatment is from 2 to 3 months.
- Phosphalugel. Contains aluminum phosphate. Removes gases in the intestines and collects toxins, harmful microelements, envelops the mucous membrane. For ulcers, take this medicine a couple of hours after eating or when pain occurs, dissolving the contents of the sachet in half a glass of water.
- Maalox. When treating ulcers, drink 1 sachet dissolved in water half an hour before meals. It is an analogue of Almagel, but its effect is 2 times longer, and it does not provoke constipation, like Almagel.
Antiemetic drugs
To alleviate the condition and eliminate the urge to vomit, the following remedies may be prescribed. Motilium. The medicine eliminates the urge to vomit. Helps improve intestinal motility, which is reflected in faster movement of food coma through the gastrointestinal tract. During treatment, short-term diarrhea cannot be ruled out.
Cerucal. The tablets inhibit the functioning of the vomiting center located in the brain. In addition, they stimulate faster gastric emptying and improve gastrointestinal motility. Metoclopramide reduces the gag reflex. After taking the drug, diarrhea does not develop.
Antispasmodics
Peptic ulcer disease is characterized by impaired intestinal motility. There are cases of both its slowdown and activation. Against the background of such a deviation, the appearance of painful cramps in the abdomen cannot be ruled out. The following are used as painkillers:
- Galidor. Taking the drug helps relax muscles, and increases vascular tone. In case of ulcerative pathology, it is used as an anesthetic drug.
- Papaverine. Taking the drug helps relax the smooth muscles of the intestines. Used for the development of pain syndrome. Contraindications for use: glaucoma, liver disease. The most common side effects are drowsiness, constipation, and allergic reactions.
- No-Shpa. The active component of the product is drotaverine hydrochloride. The drug has a selective ability to reduce smooth muscle tone, and a slight vasodilation is additionally noted. The medicine is contraindicated in severe heart failure and lactase deficiency. Adverse symptoms occur in rare cases.
No-Shpa is a popular remedy from the group of antispasmodics.
Ganglioblockers
Ganglion blockers help reduce the secretion of digestive juice, while simultaneously relaxing the smooth muscles of the stomach and gastrointestinal tract. This combination of effects provides functional rest to the ulcerated mucosa. The following medications are prescribed.
Benzohexonium
Blocks the transmission of signals from one major nerve ganglion to another. Used to eliminate the pathological symptoms of ulcers.
Dimecoline
Relieves symptoms of peptic ulcer. Has antispasmodic properties.
Kamphonium
Has powerful analgesic properties. Used to treat patients in whom the use of drugs that tonic the vascular system is prohibited. Allowed for hypertensive patients.
Quateron
It has the ability to temporarily disrupt the transmission of nerve impulses, which helps relieve pain. Additionally, treatment can be carried out with medications such as:
- Sucralfate. Forms a protective film on the surface of the mucosa, which eliminates the negative impact of aggressive digestive enzymes on damaged areas. The peculiarity of the product is that it exclusively covers the area of ulceration, without interfering with the flow of digestive processes.
- Biogastrol. Herbal medicine. The main active ingredient is licorice root extract. Its intake promotes active tissue regeneration over the entire surface of the mucous membrane of the digestive tract.
It is recommended to treat exacerbations of ulcers under medical supervision. Independent selection of medications is unacceptable, since unreasonable use of medications can cause a deterioration in the general condition.
( 1 ratings, average: 5.00 out of 5)
Treatment regimen for duodenal ulcer
Treatment according to modern principles is active drug therapy, the use of several components to draw up a treatment regimen, and a long course of medication, if indicated.
There are no fundamental differences in therapeutic regimens for gastric and duodenal ulcers; doctors adhere to the following principles in both cases:
- elimination of the causative factor;
- taking into account concomitant pathology and its adequate treatment. Drug correction should be carried out in case of pathology on the part of any organs and systems;
- the individuality of each organism is taken into account (weight, height, physical activity, possession of all self-care skills, intolerance to certain groups of drugs);
- the patient's capabilities (material well-being).
Treatment of duodenal ulcers should follow the following principles:
- etiological treatment;
- patient compliance with the prescribed treatment regimen;
- treatment with diet (special nutrition);
- mandatory drug therapy, taking into account schemes developed over the years;
- herbal medicine and treatment with folk remedies in general;
- physiotherapy methods;
- use of mineral waters;
- local treatment of ulcers that are prone to long-term persistence (do not heal).