Causes
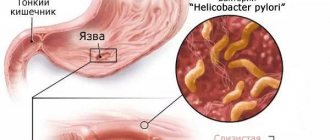
Bleeding ulcers of the stomach and duodenum always occur against the background of deep ulceration. Internal bleeding begins when the lesion reaches the vessels and arteries.
There are a number of predisposing factors to bleeding from a stomach ulcer. First of all, the occurrence of such a complication is associated with the patient’s violation of the prescribed diet. In particular, the risk increases when the patient's diet includes:
- Rough foods that can injure the ulcer.
- Hot and cold foods that irritate wounds on the mucous membrane.
- Alcoholic drinks, which are especially dangerous on an empty stomach.
- Chronic diseases of the digestive system.
In addition, a perforated stomach ulcer often occurs:
- After an abdominal injury.
- With long-term use of medications.
- For cardiovascular pathologies.
- For diabetes mellitus.
Poor blood clotting increases the risk of bleeding from a stomach ulcer. Also, defects in the mucous membranes increase with stress, nervous strain and emotional breakdowns. Sometimes a dangerous pathology can occur during heavy physical exertion or sudden lifting of weight. The following can trigger bleeding in a patient:
- Prolonged mental stress.
- Avitaminosis.
- Failure to comply with the work and rest schedule.
Sometimes doctors explain the development of a dangerous complication in a patient with gastric and duodenal ulcers by genetic predisposition. That is, if a bleeding ulcer was diagnosed in one of the adults, then there is a high probability of bleeding in the child in the future.
Hemostatic drugs
- Epsilon-amincaproic acid - reduces the intensity of blood clot resorption and activates the blood coagulation system. Administered intravenously.
- Dicynone - activates the formation of thromboplastin in the bloodstream - one of the main components of the blood coagulation system. Thanks to the production of thromboplastin, the number and activation of platelets in the vascular bed increases. The drug is able to quickly stop bleeding.
- Calcium chloride or gluconate - in contact with atmospheric oxygen, calcium ions help form a blood clot. Prothrombin is converted into thrombin under the influence of ions. The permeability of the vessel walls decreases, they begin to contract much better, which stops bleeding.
- Vitamin K activates the synthesis of components of the blood coagulation system. The action is delayed. Vitamin K will take effect 24 hours after administration.
- Fresh frozen plasma is a natural complex preparation that contains a complete set of coagulation factors. It is administered intravenously, by drip, to stop bleeding and replenish the volume of circulating blood.
- Cryoprecipitate is a balanced plasma preparation that includes the necessary coagulation factors. An effective remedy to stop bleeding from stomach ulcers.
Symptoms
If the perforation is of a hidden form, then there may be no signs of bleeding, the wound just bleeds a little. The patient's well-being changes slightly. As a rule, the only symptoms observed are weakness. But even mild, prolonged bleeding with a stomach ulcer leads to oxygen starvation of the tissues, which manifests itself in the patient:
- Dizziness.
- Headache.
- Decreased blood pressure.
- Photophobia.
In addition, if the ulcer has opened, black feces appear, and traces of blood may be observed in the belching. Symptoms of bleeding in peptic ulcer disease are more pronounced with massive blood loss.
In particular, the patient always experiences severe vomiting mixed with blood. It can be disposable or reusable, but after it there is never any relief. In this case, against the background of bleeding, the patient experiences such severe pain that the person may lose consciousness.
When the first serious signs appear, indicating severe internal bleeding, even if the body is not able to replace the blood loss on its own, the consequences of severe hemorrhagic shock are still reversible with urgent medical attention.
Otherwise, if help is not provided, symptoms of multiple organ failure may develop. This means that the patient’s blood pressure will drop to a critical level, swelling of the brain tissue will occur, and the functions of the heart and other internal organs will be weakened. In this case, a bleeding stomach ulcer can lead to death.
Symptoms of open bleeding
With hidden hemorrhage, signs are almost completely absent. The patient’s well-being practically does not suffer; there may be a slight decrease in performance and weakness.
With prolonged bleeding, symptoms of tissue oxygen starvation may occur: dizziness, pallor, headache, shortness of breath, palpitations. There may be a decrease in blood pressure when sitting or standing.
To ensure that the disease is detected in a timely manner and does not progress to a more severe stage, vomit and feces, as well as gastric juice, should be taken from time to time to carry out the Gregersen test, which allows one to detect traces of blood in the samples.
GALINA SAVINA: “How easy it is to cure a stomach ulcer at home in 1 month. A proven method is to write down the recipe. » Read more >>
First aid
When obvious symptoms appear that ulcerative bleeding has opened (blood from the mouth, anus), you need to urgently call an ambulance. It is very important to accurately describe the symptoms that caused the emergency call.
While waiting for the arrival of specialists, it is necessary to ensure that the person is completely immobile. To do this, you need to lay it on a hard horizontal surface and place a pillow under your feet. This position will increase blood flow to the brain, which will reduce the risk of hypoxia.
First aid for signs of gastrointestinal bleeding also involves cooling the stomach area to promote vasoconstriction. If you are at home, you can use ice or frozen food from the freezer.
It is necessary to apply cold for a quarter of an hour, and then remove it. This will help, if not stop the bleeding, then to slow it down to a certain extent. And this is very important for stabilizing the condition of a bleeding stomach ulcer.
It is strictly forbidden to give water and food to a person when he has an ulcer of the stomach and duodenum. This will increase gastric motility and increase blood circulation, which means blood loss will increase.
Do not give any painkillers for acute pain. You should also not try to sit the person down or lift them up if vomiting occurs. All you need to do is turn the person on their side to prevent vomit from entering the respiratory tract.
It is very important to be close to the person and constantly talk to him. We must strive to prevent him from losing consciousness. To do this, it is recommended to use ammonia before the ambulance arrives.
Bleeding from acute gastric and duodenal ulcers in clinical practice
About the article
33065
0
Regular issues of "RMZh" No. 5 dated 03/04/2009 p. 347
Category: Surgery
Authors: Siluyanov S.V. , Smirnova G.O. , Luchinkin I.G.
For quotation:
Siluyanov S.V., Smirnova G.O., Luchinkin I.G. Bleeding from acute ulcers of the stomach and duodenum in clinical practice. RMJ. 2009;5:347.
Acute erosive and ulcerative lesions of the gastric and duodenal mucosa occur in 3–4% during diagnostic esophagogastroduodenoscopy (EGDS). However, the true frequency of these mucosal lesions has not been established. Detection of acute erosions and ulcers usually occurs when patients are examined for severe symptoms of dyspepsia, but more often when complications such as bleeding occur in 60–70% of cases, or perforation in 0.5–3% of cases of acute ulcers [5, 6.10]. Often acute erosions and ulcers, complicated by bleeding, occur in patients after injuries, burns and surgical interventions [1,2,4]. Cases of detection of erosions and ulcers of the upper gastrointestinal tract after minor operations in patients who had not previously suffered from gastrointestinal diseases have been described. According to sectional data, acute ulcerations are detected in 24% of cases, and with non-selective esophagogastroduodenoscopy in 50–100% of patients in intensive care units. Mortality in gastrointestinal tract infections from acute ulcers in patients in intensive care units (ICU) reaches 80% [1,2,11]. There are various morphological criteria that make it possible to separate mucosal erosions and acute ulcers. In acute ulcers, there are deeper lesions, sometimes involving all layers of the organ wall [6]. Therefore, the incidence of bleeding of varying degrees from acute ulcers reaches 75%. In most published works, bleeding from acute ulcers is often treated as a peptic ulcer and the same treatment and tactics are applied to them. The clinical course of acute ulcers differs significantly from the manifestation of peptic ulcer disease. Uncomplicated acute ulcers are asymptomatic in most patients. The appearance of pain in the epigastric region, nausea, vomiting and pain on palpation of the abdominal wall may indicate the formation of acute ulcers and erosions of the stomach or intestines. Diagnosis of uncomplicated ulcers presents certain difficulties. Of all the known diagnostic methods, only endoscopy allows a correct diagnosis.
Acute ulcers of the digestive organs are observed at any age, both in newborns and in the elderly. The frequency of acute ulcerative lesions in old age reaches 74.6%. In the clinic of hospital surgery No. 1 of the Russian State Medical University on the basis of the Moscow City Clinical Hospital No. 15 named after. O.M. Filatov for the period 2000–2005. 745 patients with gastrointestinal bleeding from acute ulcers were treated. The average age of the patients was 59±18 years. Of these, 53.7% were over 60 years old. According to the location of acute ulcerative lesions, in 155 (21%) patients they were in the duodenum, in 590 (79%) in the stomach. It is noteworthy that in the stomach, acute ulcers were multiple in 48% of cases. When analyzing the main causes of acute ulcers, it was revealed that 356 (47.8%) patients were admitted with bleeding to surgical departments from an outpatient appointment, the rest were treated in various hospital departments. Table 1 shows the hospital units where bleeding from acute ulcers occurred. As a rule, in inpatients, the cause of gastrointestinal tract from acute ulcers was a complicated course of the underlying disease or its decompensation. In most cases, acute erosive and ulcerative lesions of the gastrointestinal tract were not prevented according to any scheme. According to the literature and our own material, based on the reasons for the development of acute ulcers, 3 groups of patients were identified: 1 – those associated with taking medications with an ulcerogenic effect (steroids, NSAIDs, anticoagulants, disaggregants, etc.); 2 – developing under stress, in the postoperative period, in conditions of organ dysfunction, in ICU patients; 3 – appearing in some acute and chronic diseases, somatic pathology, in elderly and senile patients, mainly with vascular diseases, coronary artery disease, systemic atherosclerosis, diabetes mellitus. Most patients with bleeding from acute ulcers often have all three factors that are unfavorable for the formation of complications. Figure 1 shows the distribution of patients by reasons for the formation of complications of acute ulcers. Most often in the hospital, acute ulcers were observed, appearing against the background of decompensation of certain acute and chronic diseases, often accompanying multiple organ failure syndrome (MODS). These include ulcers by T. Curling, who described acute duodenal ulcers in 10 patients with extensive burns in 1842, and H. Cushing, who in 1932 established a connection between damage to the hypothalamus and acute ulcers. T. Billroth in 1867 described observations of acute ulcers in patients with sepsis. The most common acute ulcers in this group occur with a combination of diseases of the cardiovascular system, CVD and diabetes mellitus. In more than half of the patients we observed, acute ulcers occurred due to decompensation of therapeutic or neurological pathology and grade 2-3 MODS, which corresponded to APACHE scores >15 (Acute Physiological and Chronic Health Estimation) and MODS >8 points (Multiple organ dysfunction score). When analyzing the nature of concomitant pathology, a significant relationship was found between the appearance of gastrointestinal tract from acute ulcers and the number of systemic organ lesions. In 392 (92%) patients with concomitant pathology, a combination of two or more diseases was observed, the most common manifestations were coronary heart disease, chronic nonspecific lung diseases and cerebrovascular disease. In addition, this group included 23 patients with decompensated liver cirrhosis and liver failure and 10 patients with chronic renal failure. Thus, risk factors for the development of complications from acute ulcers in this group include: • older age • decreased physical activity • 2–3 degree of organ dysfunction according to the severity assessment of APACHE, MODS Therefore, when these unfavorable factors are detected in patients, prevention of erosive and ulcerative diseases should be carried out gastrointestinal lesions. Acute ulcers associated with taking medications are observed in 45–68% of elderly patients and recently account for a third of the causes of gastroduodenal bleeding. According to our material, this is the second most common cause of complications of acute ulcers in inpatients. Most of these ulcers appear after taking cyclooxygenase inhibitors. In this group, 168 patients were over 65 years old, with cardiovascular pathology and took more than 3 medications per day, usually antiplatelet agents (acetylsalicylic acid), anticoagulants (phenindione, warfarin), NSAIDs (diclofenac, metamizole). The combination of dyspepsia symptoms with constant use of antiplatelet agents increases the risk of developing acute ulcers by 1.5–2 times. In addition, risk factors for the development of such gastropathy include: – old age; – presence of a history of ulcers; – combined or decompensated forms of concomitant diseases: cardiovascular, cerebrovascular, diabetes; – decrease in physical activity; – simultaneous use of anticoagulants, glucocorticosteroids and NSAIDs; – short, less than 1 month courses of NSAIDs and steroids. When 2 or more of these factors are combined, the risk of developing erosive and ulcerative lesions of the gastrointestinal tract increases by 2 times. In 75–90% of cases they are complicated by gastrointestinal tract. Acute ulcers in the early postoperative period develop in 2.5–24% of patients. The frequency of our observations of acute ulcers in the postoperative period was 126 (17%) patients. A relatively small number of observations of these ulcers is associated with the use of antisecretory drugs to prevent complications in risk groups in patients undergoing surgery. All acute ulcers in this group manifested gastrointestinal ulcers on days 4–9 after surgery and were observed with a complicated course of the postoperative period and progression of organ dysfunction. Risk factors for development were: – long-term artificial ventilation (more than 48 hours); – coagulopathy, disseminated intravascular coagulation syndrome; – development of severe organ dysfunction (SOD); – arterial hypotension and shock for more than 2 hours; – alcoholism; – treatment with glucocorticoids; – long-term nasogastric intubation, more than 48 hours. All these factors have I–II levels of evidence and are absolute for the prevention of stress ulcers in patients in the ICU [2,9,11,12]. It has been established that the prevention of acute ulcers reduces the risk of developing gastrointestinal tract infections without increasing the incidence of nosocomial pneumonia in the postoperative period [2,8,12]. The problem of preventing stress damage to the stomach and duodenum was discussed at the 31st Congress of the Society of Critical Medicine in San Diego (2002), at the plenum of the Russian Association of Specialists in Surgical Infections (RASHI), Imatra, 2003. There are 2 types of acute ulcers in early postoperative period: I – superficial diffuse erosions with a low risk of bleeding; II – deep localized ulcers with a high risk of hemorrhagic complications, the frequency of which in patients in the ICU reaches 14%, and the mortality rate for them is 64% [2]. The difficulties in diagnosing acute ulcers and gastric erosions lie in the fact that 60% of patients do not have clinically significant symptoms of gastrointestinal tract, the bleeding is hidden and is diagnosed only when hemodynamic disturbances appear. Diagnosis of bleeding from acute ulcers The standard in the diagnosis of erosive and ulcerative lesions of the upper gastrointestinal tract is endoscopy. With obvious clinical symptoms of gastrointestinal tract, general clinical and laboratory research methods are of diagnostic value, which, however, do not provide accurate information about the source of bleeding. During endoscopic examination, acute erosion is a superficial defect of the mucous membrane that does not extend beyond the mucosal epithelium. An acute ulcer is a superficial defect of the mucous membrane without involving the submucosal layer in the inflammatory process. Usually acute ulcers are small in size, 5–10 mm in diameter, the shape of the ulcers is round, the edges are smooth, the bottom is shallow, often with a hemorrhagic coating. Acute ulcers are characterized by their multiplicity; a combination of their localization in the stomach and duodenum is often observed. Figures 2 and 3 show acute gastric ulcers of different etiologies. Diagnosis of acute ulcers is based on medical history, clinical manifestations, endoscopy results, as well as morphological study of the mucosa. In addition to a detailed examination of the gastroduodenal zone during endoscopy, a primary assessment of the causes and nature of acute ulcers is of particular importance. In the absence of signs of active bleeding, if conditions permit, a biopsy of the mucous membrane from the ulcer areas is performed to exclude tumor lesions of the stomach. In addition, endoscopic topographic pH-metry is performed, which makes it possible to differentiate acid-peptic lesions from non-acid ones. When performing endoscopic pH-metry in patients with bleeding, the majority of subjects in all three groups found hypersecretion in areas of acid formation with a pH of less than 2 units. After performing endoscopic hemostasis in case of active bleeding, as well as in case of spontaneous bleeding, in all patients with acute ulcers, it is necessary to conduct an endoscopic assessment of the risk of recurrent bleeding according to Forrest, forming, taking into account the reasons for the formation of ulcers, groups of high and low risk of relapse. We included patients in high endoscopic risk groups for recurrent gastrointestinal bleeding from acute ulcers: • with active bleeding from one or more acute ulcers at the time of primary endoscopy F IA, F IB with any severity of blood loss or anemia, there were 105 of them in our observation (14, 1%); • with bleeding F IIA, F IIB with moderate or severe blood loss or anemia, 240 (32.2%) of such patients were identified. In these groups of patients, either endoscopic hemostasis or endoscopic prevention of recurrent GIB was required, as in patients with chronic ulcers. In the remaining 53.7% of patients with F IIC, F III, with clinical manifestations of bleeding, regardless of the severity of anemia, a low risk of recurrence of gastrointestinal tract bleeding was stated. Based on the results of primary gastroscopy in groups at high risk of recurrent gastrointestinal bleeding, dynamic studies in patients are necessary for endoscopic prevention of recurrent hemorrhage. The timing of repeat endoscopy depends on the reliability of the primary hemostasis performed; on average, it is 1–3 days from the first study. During dynamic endoscopy, the risk of recurrence of gastrointestinal bleeding is re-evaluated and its prevention is carried out if the threat persists. In the later stages after hemostasis, repeated endoscopy is used to assess the results of ulcer healing or their chronicity. Usually 7–10 days are enough for the picture of scarring of ulcers to be observed against the background of elimination of the main factors of erosive and ulcerative lesions. If this does not happen, in 10–12% of patients, acute ulcers may become chronic with the appearance of signs of the formation of an inflammatory shaft, their deepening and repeated complications. An example of the progression of an acute ulcer during treatment is presented in Figures 4 and 5. When the ulcer becomes chronic on repeated endoscopy, the treatment tactics should be the same as for peptic ulcer disease, i.e. repeated relapses of bleeding are indications for surgical treatment. Therefore, such patients in the study should use methods such as radiography of the stomach, traditional intragastric and daily pH measurements, as well as further clinical observation as for peptic ulcer disease. Prevention and treatment of bleeding from acute ulcers The main method of treating bleeding from acute gastrointestinal ulcers is currently endoscopic hemostasis. The outcome of treatment of patients with acute ulcers largely depends on the success of this stage. In 640 (86%) patients, bleeding was present at the time of examination, in 105 (14%) it was active, which required endoscopic stop during the initial examination. Injection methods were used in the form of periulcerous administration of an alcohol-novocaine mixture, thermal electrocoagulation, argon plasma coagulation, laser coagulation, and microwave coagulation. In case of active bleeding, combined methods of hemostasis were predominantly used, combining injection and thermal methods. When bleeding occurred in patients at high risk of relapse, endoscopic prevention of gastrointestinal tract recurrence was carried out using one or more of the listed methods. In patients with F IIB, the condition for effective endoscopic hemostasis is the removal of a blood clot from the ulcer using a washout or a loop, followed by prevention of relapse or stopping active bleeding. With a low risk of relapse among 400 patients, only 120 (30%) received relapse prevention, which may subsequently serve as one of the reasons for recurrent bleeding in this group. Primary endoscopic hemostasis was successful in all 105 patients with active bleeding; a combined hemostasis method was used in all of them. In the group at high risk of relapse, endoscopic control of hemostasis was carried out, and control endoscopy was performed 1–5 days after the initial examination. At each endoscopy, the quality of hemostasis, the risk of recurrent bleeding was assessed, and prophylaxis was carried out using all of the above methods. With successful endoscopic hemostasis, further methods of prevention and treatment are: antisecretory and gastroprotective therapy aimed at maintaining the pH in the stomach above 6 units. most of the time of the day, normalization of the motor-evacuation function of the stomach, increasing the resistance of the mucous barrier. For the prevention and treatment of acute ulcers, the following are currently used: antacids, H2 receptor antagonists and proton pump inhibitors (PPIs), gastroprotectors. Of all the groups of drugs for the prevention and treatment of gastrointestinal tract, today proton pump inhibitors (PPIs) best meet all the requirements of modern antisecretory therapy and are recommended by the International Association of Gastroenterologists for the treatment of a number of acid-related diseases. PPIs have a much stronger and longer-lasting antisecretory effect compared to H2 receptor blockers [3,7,13]. It is very important for the treatment of ulcer bleeding to have not only tablets, but also parenteral forms of these drugs. Therefore, they are optimal for the prevention of the formation of acute gastrointestinal ulcers and the treatment of their complications. To assess the effectiveness and necessity of antisecretory therapy for acute ulcers with gastrointestinal tract on days 3–5 after primary hemostasis in stable patients, we used intragastric pH-metry. It was assumed that hydrochloric acid and pepsin, when bleeding has developed, inhibit thrombus formation and cause lysis of already formed blood clots. Vascular-platelet hemostasis occurs only at pH values above 6 units. We compared antisecretory therapy in patients with acute ulcers during treatment with H2 blockers and pantoprazole (Controloc 40 mg). Examples of the action of intravenous famotidine and intravenous Controloca, with daily pH measurements, are presented in Figures 8 and 9. As can be seen in the pH grams, the use of pantoprazole made it possible to maintain pH
Diagnostics
An experienced emergency specialist, even during the initial examination with little blood loss, can determine from characteristic symptoms and signs that blood is leaking from the ulcer. But in order to determine the extent of the bleeding ulcer and the danger of the resulting complication, it is necessary to accurately establish the diagnosis. To do this, you need to take tests and perform a number of studies:
- General blood analysis. In it, the main indicators for confirming bleeding will be a decrease in the number of red blood cells and hemoglobin.
- Coagulogram, which determines blood clotting.
- Bilirubin test. The level of this substance always increases with perforation and perforation of the ulcer.
- Ultrasound of the abdominal cavity.
If the patient’s condition allows, then after his admission to the hospital, diagnosis of a bleeding gastric ulcer is carried out using endoscopic examination. During the procedure, the mucous membrane of the digestive organ is examined using a special probe. This allows you to determine the exact location of the bleeding.
An open stomach ulcer often causes severe bleeding. As a result, obvious symptoms arise that do not require additional diagnostics. In this case, measures are taken to stop the bleeding. Sometimes surgery is urgently required.
Traditional treatment and surgery
The patient is hospitalized in the surgical department. Here the diagnosis of the disease is carried out. In case of large blood loss or serious condition, the patient is sent to the intensive care ward or intensive care unit.
Urgent measures
Emergency therapy and bleeding control are carried out immediately after the patient is admitted to the hospital. The following activities are carried out:
- Intramuscular injection of Vikasol.
- The substance calcium chloride, aminocaproic acid, is injected into the vein.
The measures help stop bleeding and prevent blood clot formation.
First stage
Internal bleeding is controlled using an inflatable balloon catheter. It is introduced into the patient's mouth. The balloon is inflated with air. It squeezes the vessel. Chemical sclerosis stops bleeding.
Endoscopic therapy
During the procedure, the ulcer is cauterized, which bleeds. To do this, a special substance is injected into the patient’s vein, which increases blood clotting.
The operation is performed in cases where therapeutic measures have not given a positive result.
Mechanical therapy
Extensive bleeding is eliminated in the following ways:
- Suturing the ulcer and the affected vessel.
- Clipping. The location of the bleeding is determined using an endoscope. Special clips are placed on the vessel. The method is used for bleeding from varicose veins.
- Angiographic embolization. Microscopic spirals are inserted into the lumen of the affected vessel.
- Gastric resection. The operation is performed in cases where previous methods do not have an effect. The ulcerative lesion is excised to the borders of healthy tissue. The stomach is sutured.
Surgery requires a long recovery. The patient is on strict bed rest.
After discharge, the patient is registered at the dispensary. The gastroenterologist monitors the patient's condition. He conducts periodic courses of therapeutic treatment.
Treatment of bleeding from stomach ulcers
At the slightest suspicion of the presence of a bleeding ulcer, emergency hospitalization of the person is carried out. Treatment for bleeding gastric ulcers begins with strict bed rest and complete abstinence from food.
The goal of all procedures is to stop bleeding in the stomach. Treatments are carried out under the mandatory supervision of a doctor. The effectiveness of treatment for bleeding gastric ulcers is evidenced by the improvement in the patient's condition.
Treatment of gastric ulcers involves emergency hemostatic therapy. Once the patient's condition has stabilized, a strict special diet will be prescribed.
If a large loss of blood occurs during gastric bleeding, a blood transfusion will be required. This procedure is also necessary if the bleeding cannot be stopped in a short time.
Advice! It is unacceptable to conduct an examination and prescribe treatment to stop ulcer bleeding on an outpatient basis.
Drug therapy
To stop gastric bleeding, it is necessary to carry out drug therapy for the stomach. For this purpose, drugs are used that can stop bleeding. This:
- Aminocaproic acid. It promotes vasoconstriction and increased blood clotting. The product is also able to suppress specific allergic reactions. In addition, the drug helps remove toxins from the body.
- Vikasol. This is a chemical analogue of vitamin K, which normalizes blood clotting.
- Calcium chloride. The drug reduces internal bleeding and can be used as an antiallergic agent.
To restore the water-salt balance during internal bleeding, special solutions are prescribed. The most famous are rheopolyglucin and trental.
Advice! In the process of treating a bleeding stomach ulcer, painkillers can be used, but they should be prescribed by a doctor taking into account the patient's condition.
Operation
Today, a large number of effective methods of endoscopic hemostasis have been developed to eliminate bleeding in the stomach. The most commonly used are thermal effects, which involve cauterization of a bleeding ulcer. For this purpose the following is used:
- Electrocoagulation.
- Laser coagulation.
- Argon plasma coagulation.
- Radiofrequency coagulation.
- Thermal probes.
- Suturing an ulcer.
Injection treatments using endoscopy involve the administration of various medications to deliver them directly to the lesion. It is also common to perform clipping or ligation of bleeding vessels during gastroduodenoscopy.
Hemostatic materials, such as biological glue and hemostatic powder, can be used. If conservative and endoscopic treatment methods are not effective, then surgical treatment is always considered.
Surgery is indicated for elderly patients who have experienced gastric bleeding. This is due to the fact that most drugs whose action is aimed at eliminating bleeding have age-related contraindications and their use can cause unpredictable consequences. Other indications for surgery are:
- Massive bleeding.
- Regular relapses.
- The location of the defect is near large arteries.
The operation involves performing a gastric resection under general anesthesia. In this case, the affected area is completely excised, and the walls of the stomach are stitched. After such an operation, long-term rehabilitation is required.
Diet
In the first 2-3 days with a bleeding stomach ulcer, you must completely stop eating. Extreme thirst can be relieved with ice cubes or a spoon of water. As a rule, after this period the condition can be stabilized.
Therefore, after bleeding, you can start eating small amounts of liquid food. The diet for stomach ulcers in this case involves the gradual inclusion of the following products in the diet:
- Raw from soft-boiled.
- Milk.
- Milk and oatmeal jelly.
- Not strong jelly.
- Sweet diluted juice.
It is very important that all food is taken in small portions, but quite often. When the condition stabilizes, nutrition for stomach ulcers should become more varied. Other dietary dishes should appear on the menu. It can be:
- Carrot and mashed potatoes.
- Slimy soups.
- Puree porridge.
- Meatballs steamed from lean meat and fish.
- Curd mousses and soufflés.
- Cream.
It is allowed to season dishes with a small amount of butter and vegetable oil. It is very important to use fresh and high-quality products for preparing dishes. Sometimes you are allowed to drink weak tea with milk, as well as a decoction of rose hips and sweet compotes.
This diet must be followed for a long time to avoid relapses. It is strictly forbidden to consume alcoholic and carbonated drinks, any sour foods, dishes with added spices, strong tea and coffee.
Advice! Any changes in diet should be discussed with your doctor.
Treatment
For bleeding gastric ulcers, therapy is performed in an intensive care unit or inpatient department. Elimination of blood loss is performed using conservative methods. Competent medical care is used to stop blood loss. To prevent bleeding, it is important to prevent the possibility of recurrence. First of all, the patient is hospitalized. At the initial stages, solutions of sodium chloride and epsilon-aminocaproic acid are administered intravenously. These drugs allow you to achieve the desired hemostatic result and resist the development of ulcers. Stabilized hemostasis prevents complications and death.
In cases of massive bleeding, surgery may be required. To stop the complication of a stomach ulcer, red blood cells are injected into the patient's body. It helps maintain the balance of red blood cells in the bloodstream and avoid increasing anemia. Therapy depends on the location of the lesion and the severity of the symptoms of the pathology. Therapeutic treatment of gastric ulcers with bleeding includes the use of special agents that promote blood clotting. Therapy aimed at arterial fibrosis is often used.
First aid
When bleeding from a stomach ulcer you must:
- provide the patient with complete rest;
- lay the victim down and raise his legs;
- put an ice pack on your stomach;
- call an ambulance.
Providing the necessary first aid should be carried out clearly and competently. No medications should be given. In case of loss of consciousness, it is necessary to monitor respiratory function and pulses. If necessary, perform cardiac massage and artificial respiration. When your stomach hurts and your stomach ulcer is bleeding, the emergency doctors will tell you what to do.
Drug therapy
Treatment of patients includes the use of:
- antibacterial drugs (Vicalin, Furazolidone, Amoxicillin);
- histamine receptor blockers and antisecretory drugs (Piloride, Famotidine, Ranitidine);
- proton pump inhibitors (Pariet, Rabeloc, Omeprazole);
- antacids (Keal, Almagel, Maalox);
- antispasmodics (Papaverine, No-shpa, Drotaverine);
- probiotics (Bifiform, Linex, Lactiale).
The doctor prescribes a treatment regimen individually, taking into account the symptoms and nature of the pathology. Therapy with conservative methods is aimed at eliminating pathogenic flora, increasing blood clotting, stabilizing the digestive functions of the stomach, pain relief and healing of the affected area.
Surgery
Particular attention is paid to surgical treatment of peptic ulcer. In some situations, bleeding stomach ulcers require surgery. Various surgical techniques are performed:
- sclerotherapy;
- endoscopic electrocoagulation;
- embolization of the intestinal artery;
- selective catheterization with the introduction of Vasopressin.
Surgical treatment is performed when conservative methods fail to achieve the desired therapeutic result. The operation is indicated for patients both at the height of bleeding and in the intermediate period.
When internal bleeding occurs during an ulcer, the blood loss can be very voluminous. Elimination of bleeding from an open stomach ulcer requires the presence of donor blood. The surgeon identifies existing damage and repairs it, stopping blood loss.
Diet and nutritional habits
During the recovery period, diet and nutritional habits play a special role. The therapeutic diet includes eating low-fat foods that are easily digestible. Recommended to eat:
- oatmeal jelly;
- scrambled eggs;
- cream;
- vegetable puree.
Meat dishes are included in the menu later in the recovery period.
Complications
If an open bleeding ulcer is not completely cured, this means that the bleeding will not be completely eliminated. Against this background, there are high risks of relapse. Even minimal blood loss can significantly worsen the patient's condition and cause very dangerous complications, reduce survival and increase the risk of death.
If a bleeding ulcer is not treated properly, anemia may develop. This is a very dangerous condition, which leads to an increase in weakness, provokes dizziness and subsequently a complete loss of performance.
Symptoms of developing anemia include, in addition to a deterioration in general well-being, the appearance of a grayish tint on the skin and paleness of the mucous membranes. Very often the patient experiences numbness in the lower extremities.
An increase in temperature may occur periodically. As a rule, due to increased weakness, the pulse increases significantly when moving. A complication of a bleeding ulcer can be a disorder of all body systems, in particular liver dysfunction.
This is very dangerous, as this results in toxic poisoning of the body and metabolic disorders. The most terrible complication of an untreated bleeding peptic ulcer due to constant blood loss is cerebral edema.
These are not all the dangerous consequences that can result from incorrect diagnosis and incorrect treatment. Statistics show that the mortality rate from hemorrhage is 10-15%, and in cases where massive bleeding occurs, 50-55% of patients cannot be helped.
Why does bleeding occur?
Gastric and duodenal ulcers with bleeding are a dangerous pathology. What can cause bleeding? Experts divide all the reasons into several groups:
- mechanical (frequent and excessive consumption of foods enriched with coarse fibers);
- thermal (frequent and excessive consumption of hot or very cold food);
- chemicals (some substances can cause damage to the structure of stomach cells and thus bleeding: alcohol, caffeine, tobacco, etc.);
- pharmaceutical (long-term therapy with certain medications, for example, Aspirin, Ibuprofen, Naproxen, etc.).
As the disease progresses, it damages and destroys a large number of blood vessels, which causes bleeding.
Prevention
To prevent bleeding stomach ulcers, you should take care of your health. It is very important to prevent the occurrence of pathology if a chronic ulcer was previously diagnosed. To do this, you need to promptly treat any diseases of the digestive system.
It is also important to eat right, avoid stress, minimize nervous tension, and also eliminate increased mental and physical fatigue. It is important to learn how to properly organize your work and rest schedule. It is recommended to undergo regular medical examinations and, if any pathological changes are detected, to follow all doctor’s instructions.
But even if a stomach ulcer is diagnosed, it is important not to get upset prematurely. Today there are many ways and methods of successfully treating the most complex forms of the disease. It is important to continue to lead an active lifestyle and follow a strict diet while completely abstaining from alcoholic beverages and smoking. Refusal of treatment threatens the death of the patient.
A positive prognosis for treatment of a bleeding stomach ulcer largely depends on the correct attitude of the patient. The main thing is to believe that you will be able to defeat the disease and do everything for this.
Causes
Often it is not possible to determine the cause of ulcer bleeding. It is not suitable for such provoking factors as physical or mental stress, mental trauma, violation of the integrity of the abdominal cavity, or others.
Gastric bleeding is often associated with the occurrence of a necrotic process during an exacerbation of the disease, as a result of which the integrity of the vessel is disrupted.
Sometimes atherosclerosis is the main cause of the complication. Gastric bleeding is promoted by vitamin deficiencies, thrombosis or other diseases of the vascular network. The process can be triggered by a previous infectious disease or a dietary disorder. Alcohol and smoking can affect the likelihood of blood loss.